November 17 was World Prematurity Day. I know first hand how stressful it is to have a premature baby: three of my children were born prematurely and needed special care in the Neonatal Intensive Care Unit (NICU).
When my first child was born at only 30 weeks and five days gestation, I knew little about preterm babies or breastfeeding. Our NICU experience ignited my passion for maternal and infant health, and I’ve since become a nurse and a lactation consultant. I wanted to share my experience of caring for my own premature babies, as well as many others.
Premature babies need special care
Compared to full-term babies, premature babies need more support and less handling and stimulation. With my first, I felt like I couldn’t do much for him in the NICU, but I learned that I could still change his diapers, do mouth care, and do belly button care.
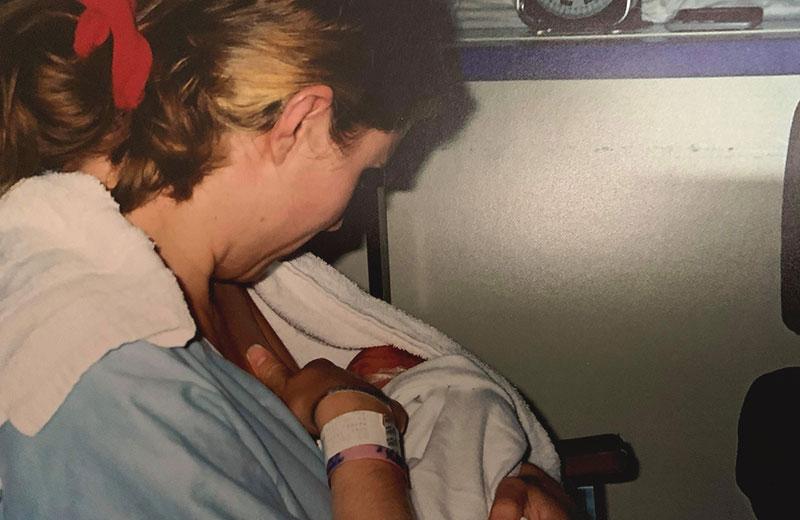
Our pediatrician also talked to us about the importance of skin-to-skin care, or "Kangaroo Care." I would get a water bottle, some snacks, a book, and I would sit down and hold my baby in this way for about two hours. This was vital for his health and our bond, and helped to reduce how much he was handled.

Preparing NICU babies for feeding
Typically, babies don’t eat by mouth until they are at least 33 weeks old; younger babies don’t yet have the suck-swallow-breathe coordination. Before he was old enough, I would hold my son skin-to-skin on my chest while he was being tube fed, and in this way, he could start to connect his full tummy with being at the breast or chest, skin-to-skin. Babies can also nuzzle at a "dry" breast (that has been pumped to limit milk flow). At about 33 weeks, I noticed him cueing to feed, like when he licked his lips.
Expressing milk – from drops to full feeds
Breast milk for preterm babies is specially designed to meet their needs, so I started expressing my milk on day two after my son’s birth. With premature babies, there can be delays in milk "coming in" - mine didn't come until day five. It was so discouraging to pump every two-to-three hours to only get about 1mL. The nurses would capture this early milk (colostrum) with a Q-tip and use it for his oral care, but it was hard for me to keep going when I didn't feel like I was getting any results.
Then, on day five, I started to notice about 5mL - it was so exciting! From there, bit by bit, my milk increased until I was meeting his needs and able to put some extra in the freezer.
Discovering the art of breastfeeding
My goal was to feed my son at the breast, but it wasn't easy! Everyone around me was telling me something different. Ultimately, I learned that breastfeeding is an art, and that they were giving me tips for things to try. I had to learn about my baby and what would work for us.
There were highs and lows while he was learning to feed. I would see him sucking and it seemed like a good feed, but then he might only gain a couple of grams in weight. We stuck with it and, after about three to four weeks, breastfeeding was going well and he was taking most of his feeds at the breast.
Tips for breastfeeding
By the time I had two more premature babies, I knew a lot more about feeding them. Now, when I work with parents in the NICU who want to breastfeed, I encourage them to:
- Start skin-to-skin right after birth, as soon as baby is medically stable.
- Avoid or delay using bottles.
- Learn the difference between nutritive and non-nutritive suckling (you can think of non-nutritive suckling as "practicing" for breastfeeding).
- Use breast compressions, which can get milk into baby's mouth even if they are not doing nutritive suckling.
- Move more milk with "hands-on pumping," which can include breast massage, breast compressions, and hand expression.
- Feed or express milk regularly, including at night, if full breastfeeding is the goal.
- Focus on things other than the numbers: Did the latch feel good? Was baby having a good feed? What was baby sharing through their cues?
In sharing this story, my goal is to give readers hope that breastfeeding premature babies is possible. To learn more, check out the following resources:
- Kangaroo Care: Information for parents (PDF) - Perinatal Services BC
- Breastfeeding your preterm baby (PDF) - Perinatal Services BC
- Breastfeeding and human milk - Northern Health













Comments