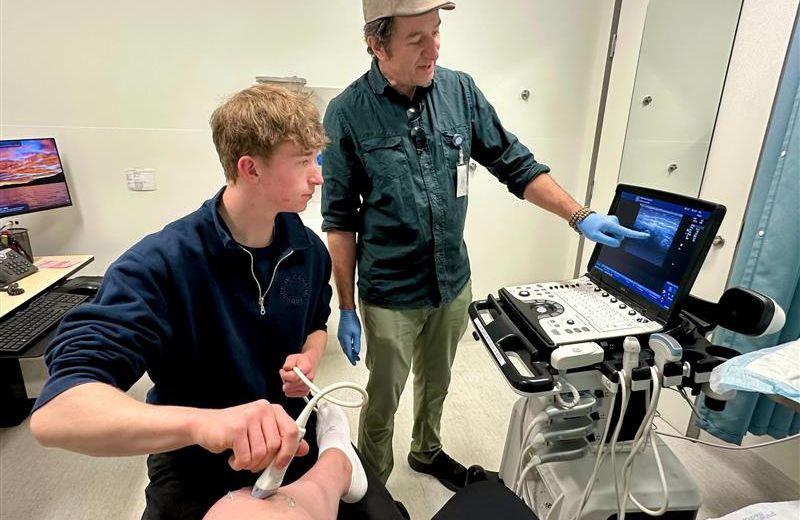
On Haida Gwaii, Northern Health’s most western Health Service Area (HSA), local physicians are transforming patient care through the innovative use of point-of-care ultrasound (POCUS)—a technology that’s proving to be a game-changer for rural medicine.
POCUS allows clinicians to perform real-time imaging at the bedside, enabling faster diagnoses and more immediate treatment decisions. For communities like Haida Gwaii, where access to advanced imaging and specialist care often requires costly and time-consuming travel to the mainland, this tool is more than just convenient—it’s essential.
Dr. Tandi Wilkinson, one of the lead authors of the full article (attached) and a long-time advocate for rural health innovation, emphasizes that POCUS is not just about technology—it’s about equity. “When we can diagnose a life-threatening condition like an ectopic pregnancy or heart failure right at the bedside, we’re not just saving time—we’re saving lives,” she notes.
The success of the Haida Gwaii model lies in its sustainability. Rather than relying on short-term training or external experts, the community has built a self-sustaining ecosystem of learning. Local physicians receive ongoing mentorship, participate in peer-to-peer learning, and have access to a growing library of case studies and protocols tailored to rural practice.
This grassroots approach is already showing results. Emergency room visits are more efficient, patient satisfaction is up, and the health care team reports greater confidence in managing complex cases. Perhaps most importantly, patients no longer need to leave their community for care that can now be delivered safely and effectively at home.
The story of Haida Gwaii’s ultrasound initiative is a powerful reminder that innovation, a core value Northern Health often celebrates, doesn’t always mean high-tech or high cost. Sometimes, it’s about rethinking how we use the tools we already have—and empowering local teams to lead the way.
As rural and remote communities across Canada continue to face challenges in accessing timely, high-quality care, the Haida Gwaii experience offers a hopeful blueprint. With the right support, training, and vision, small communities can lead big changes in health care.
If you’d like to read the Doctors of BC full publication on POCUS, which this story was based on, check out Innovative use of point-of-care ultrasound improves health care on Haida Gwaii.













Comments