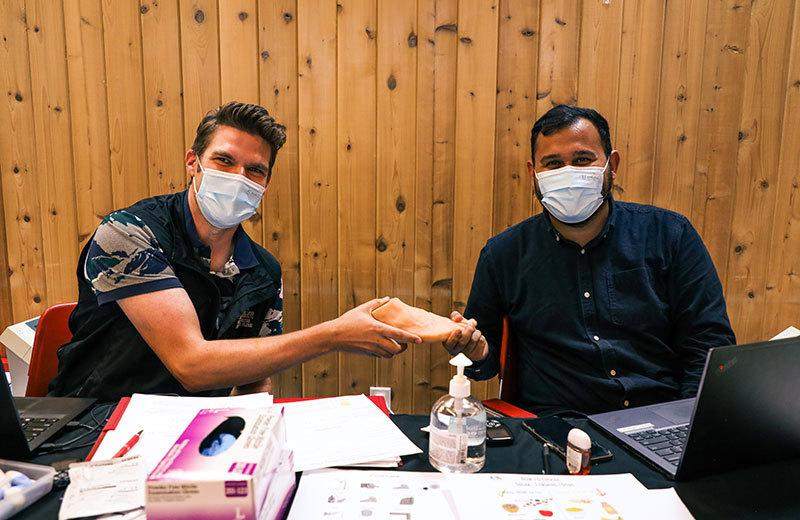
The Mobile Diabetes Telemedicine Clinic (MDTC) (a partnership between First Nations Health Authority, Carrier Sekani Family Services, and Northern Interior Rural Division of Family Practice) is a travelling service that supports diabetes prevention and intervention education across Northern BC. They provide on-site lab analysis, health education, telehealth, and annual chronic care recommendations to hundreds of First Nations people. This model has enabled people to gain access to care and wellness streams that have led to improved health outcomes. The addition of a Primary Care Network (PCN) diabetes nurse has further strengthened access to ongoing primary care, as it allows for dedicated outreach within the clinic.
A focus on patient-centred care
An example of the benefit of this service can be seen in the care one woman with high-risk gestational diabetes received from the PCN diabetes nurse. Gestational diabetes, which presents as high glucose in the blood during pregnancy that usually ends after birth, can present challenges, especially if the patient is unaware of their diagnosis. The PCN diabetes nurse was sensitive to the risk factors and acted with great respect for this patient and their individual circumstances. The nurse took several important steps. They:
- Maintained regular contact with the patient, which helped build the patient’s confidence that their health and the heath of their baby was important.
- Maintained regular contact with the patient’s primary care provider.
- Measured and adjusted insulin daily for the patient.
- Helped the patient get a continuous glucose monitor, which allowed the nurse and patient to keep in close contact, to monitor glucose levels, and prevent problems.
- Discussed additional support measures (such as food choices, physical activity, stress management, and housing concerns).
- Advocated within their professional role to help the patient set up much needed supports in their personal life.
These conversations and steps helped the nurse build a trusting relationship with the patient. Because of the relationship and the trust that grew from it, the patient asked that their diabetes nurse discuss the birth and postpartum (after birth of the baby) plan with the patient’s doctor.
Building trusting relationships supports better patient outcomes
Through compassionate, preventive, and localized care, the MDTC and PCN diabetes nurse helped to foster in the patient a level of trust in the medical system. The patient continues to have close contact with this nurse in their postpartum care. The relationship minimized the immediate risks to both the patient and baby during pregnancy, birth, and postpartum, and also helped reduce the patient’s risk for future problems associated with diabetes.
Collaborative programs like this one, where the MDTC and the PCN nursing staff work together, are invaluable. The quality of care and outreach made possible by the program helps prevent hospitalizations, related complications, family hardships, and possibly deaths. Building relationships through compassionate care helps to build and/or rebuild trust in the health care system.
Learn more about the MDTC and the work they do.













Comments