COVID-19 has had a tremendous impact on health authorities and patients around the world. It’s hard to imagine the experience a patient goes through when the unthinkable happens and they are hospitalized. In some cases, patients require ventilators, a machine that provides mechanical ventilation by moving breathable air in and out of the lungs.
In April 2020, a patient who had been hospitalized and on a ventilator due to COVID-19 was asked what could have been done to create a better experience given the circumstances. The patient informed the staff member that communication with the care team was difficult while connected to a ventilator. This feedback was sent to Northern Health staff members Beth Ann Derksen, executive lead for Critical Care, and Jeanette Foreman, NW quality improvement lead.
From there, staff started collaborating address the feedback. Jeanette conducted some initial research and then reached out to Julie Lidstone, chief speech-language pathologist at the University Hospital of Northern BC (UHNBC), to assist in developing something to support patient communication. Julie engaged UHNBC speech-language pathologists (SLP) Pamela Ross and Sophia Neppel, as well as Ashley Lequereux, an SLP with Communication Assistance for Youth and Adults (CAYA), to participate in the initiative. SLPs are highly-educated professionals who specialize in the evaluation, diagnosis, and treatment of speech, language, voice, and swallowing disorders.
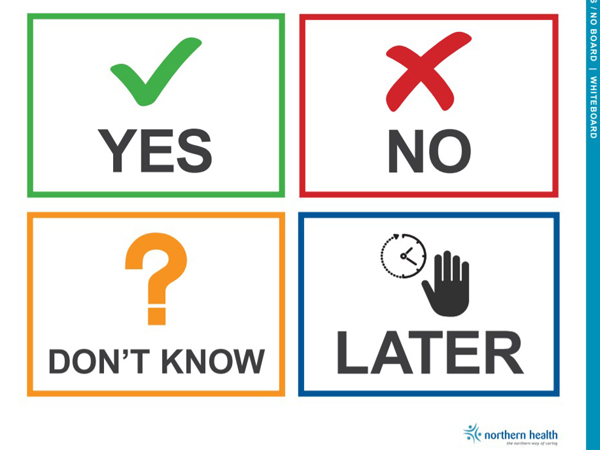
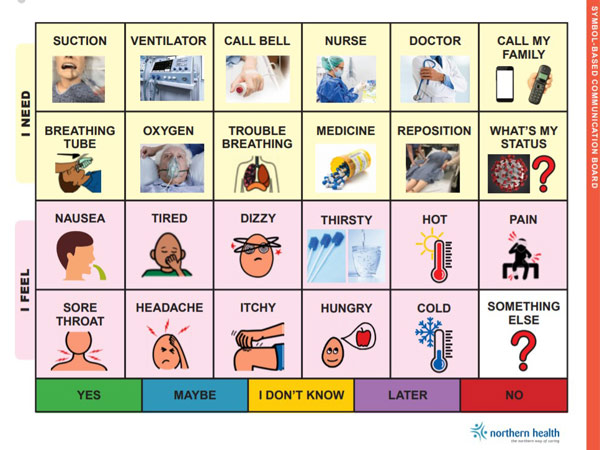
Next, Julie, Pamela, Sophia, and Ashley worked with nursing leaders to design a toolkit consisting of a set of communication boards. The boards let patients communicate their needs by gesturing or pointing at letters, pictures, and common words and phrases, as well as writing messages. Various evidence-based communication boards were reviewed to create the toolkit.
The SLPs also connected with colleagues across various programs and sites to gather information and review the design of each board. Although Northern Health and other health authorities have general communication boards to assist patients in communicating, they needed one that was specific to patients in the intensive care unit (ICU).
“I was happy that the Speech-Language Pathology Department was able to participate in this project and provide a means of communication for this patient population,” says Pamela. “I’m very proud of our team and the help that we were able to provide during this time.”
Pamela had recently completed her certification in the CAYA Partners program, which provides additional training to SLPs working in the area of augmentative and alternative communication (AAC). Along with Ashley’s expertise, as the CAYA representative in the North, they provided a strong foundation for development of this communication toolkit. CAYA is a province-wide service program that supports youth and adults aged 19 years and older, with assessment and intervention in the area of AAC.
The team was able to create the communication toolkit in only a couple of weeks. On April 29, 2020 the Intensive Care Unit (ICU) Assisted Communication Toolkit was approved, printed, and distributed to each ICU across the organization. Pages were laminated to ensure it could be sanitized between patients and to follow infection control standards.
“I was thrilled that our team had the opportunity to participate in this initiative,” says Julie Lidstone, chief speech-language pathologist. “The ability to communicate is not only the patient’s right, but is essential to providing patient-centered care. It is instrumental that patients have the opportunity to participate in their care.”
The development of the ICU Assisted Communication Toolkit is another example of Northern Health’s person- and family-centred care focus. Although its original purpose was to increase communication for ICU patients during the COVID-19 pandemic, the ICU Assisted Communication Toolkit can also be used to facilitate communication for a broad range of patients. The toolkit will increase opportunities for better communication, assist in reducing patient and provider frustration and help to improve overall health outcomes.














Comments