Since 2012, the Northern Clinical Simulation program has been a partnership between Northern Health, the Northern Medical Program, and the University of Northern BC's School of Nursing. It was developed to provide high-quality hands-on training to Northern communities.
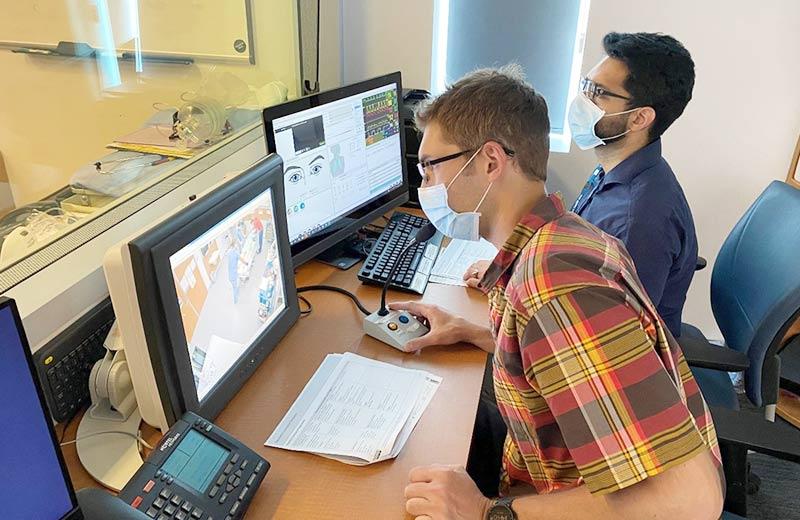
The program uses life-sized, anatomically correct mannequins, known as "simulators" to provide realistic training for health care professionals. The simulators – which can breathe, speak, and bleed – provide practise in dealing with births, hemorrhages, broken limbs, heart attacks, and more. This lets health care professionals get hands-on skills, practising as a team and without risk to patients.
One particular group that this program has helped support is family practice residents in the North.
When students finish medical school, those choosing to specialize in family medicine must complete an extra two years of training. This includes in-hospital training, as well as work in a community family medicine clinic. They can also attend simulation sessions to increase their hands-on experience with various health emergencies and acute care scenarios.
"The program is very valuable," says Dr. Matthew Wahab. "Simulation, in general, has been used as a teaching tool in other industries for a long time. The program creates a safe environment that helps identify learning gaps and teaches residents how to apply their knowledge in the heat of the moment".
Three years ago, Dr. Wahab completed the UBC Family Medicine residency program in Prince George and believes that the integration of simulation into the curriculum is crucial to the development of physicians who practise acute care medicine in both urban and rural settings. The simulation program has also been shown to improve patient safety and reduce health costs.
In recent years, through the support of the Northern Clinical Simulation program, family practice trainees have developed several successful simulation-based research projects focused on improving the quality of education for student residents and rural physicians.
The first project, supervised by Dr. Brydon Blacklaws, helped create a refresher course for incoming resident physicians geared towards on-call emergencies. This well-received project created a smoother transition to practice.
A second project, supervised by Dr. Floyd Besserer, involved the development of a simulation curriculum of acute care scenarios geared towards rural sites in the North. Physicians were happy to see this being put in place, as demand for more simulation in rural hospitals and health care centres has increased.
"I would like to credit Michael Lundin, regional manager [of] Clinical Simulation Education; the simulation centre staff; and the affiliated partners on providing us with the opportunity to use the simulation labs,” says Dr. Wahab. “Without them, none of this would happen."
In the future, Dr. Wahab hopes to see more integration between residents and medical students. He’d also like to see simulation used as a longitudinal metric for competency-based medical education.
More information and donations
Visit the Northern Clinical Simulation page for more information.
In recent years, significant support from the Spirit of the North Healthcare Foundation and its donors has allowed the program to buy newborn and one-year-old simulators that resemble real infants. This has made it possible for health care professionals to safely practice providing care to this age group. However, more help is needed: donate today.













Comments